We are back up here again, with another pleural effusion.
To keep myself from seeming redundant, I'll answer the questions we've been getting the most of, quickly, and as short as I can.
-No, it's not as bad as the last few.
-No, we didn't bring him up here suspecting this. We brought him to a pediatrician at the U because he's had a cough and Josh had had pneumonia. But they wanted an x-ray which is how we discovered it.
-No, the Doc's don't know why it happened again, and they are concerned, but they aren't going to do anything drastic at this point (like a cath,) because it could be the cold that is associated with this episode.
-Yes, Jack is pissed.
-Yes, we are about through with the novelty of pleural effusions.
-Yes, Tom and Becky are back. They are home recovering from a bad flight, long trip and exhaustion. They'll come up tomorrow.
-No, we don't need anything right now.
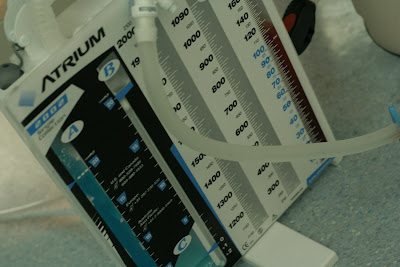
-Yes, they put in a chest tube, it will be in for a day or two.
-Yes, we will keep him on diuretic's for a longer time now.
-Yes, we are worried about the potassium levels.
-Yes, they'll have to draw his blood every morning before an x-ray.
-Yes, I'll be spending each night here that he needs to be here.
-No, we hope this won't happen again.
So my theory, is that last week when we took his diuretic down to once a day, Jack began to get sick and like any mother would- I gave him "lots of fluids" to help his cold. So we bumped UP fluids after bumping DOWN diuretics which probably didn't help, and Jack has been doing alot of violent coughing which I'm sure aggrivates the area around his lungs and doesn't help either.
So here we are again. People recognize us now, nurses know our routines and what we like and don't like. Our cardiologist is going out of town and I hope all these people I haven't worked with before know what they are doing, and who they are dealing with. We are hoping to be out of here by the weekend, so we don't have to tack on Father's Day to our stays here during Easter, Mother's Day, and Josh's Birthday.
Thanks to those who are praying, and thanks to those who have expressed their concerns today. We love and appreciate you all.